An operational approach to National Institute on Aging-Alzheimer’s Association criteria for preclinical Alzheimer disease.
OBJECTIVE
A workgroup commissioned by the Alzheimer’s Association (AA) and the National Institute on Aging (NIA) just lately revealed analysis criteria for preclinical Alzheimer illness (AD). We carried out a preliminary evaluation of those pointers.
METHODS
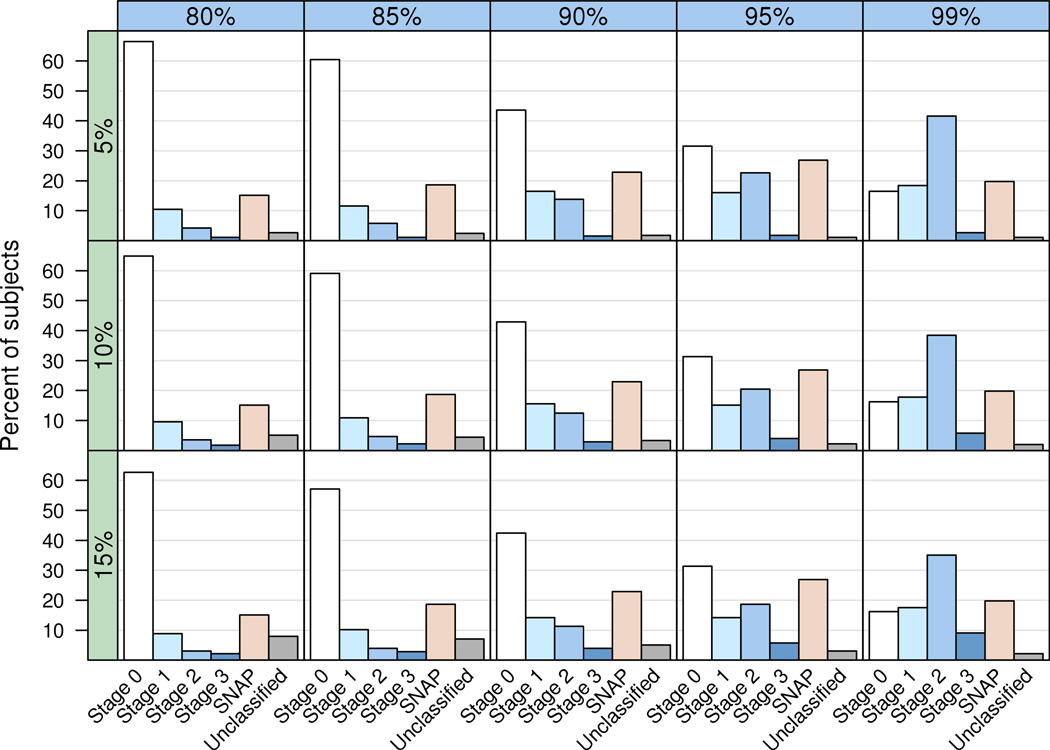
We employed Pittsburgh compound B positron emission tomography (PET) imaging as our biomarker of cerebral amyloidosis, and (18) fluorodeoxyglucose PET imaging and hippocampal quantity as biomarkers of neurodegeneration. A gaggle of 42 clinically identified AD topics was used to create imaging biomarker cutpoints. A gaggle of 450 cognitively regular (CN) topics from a population-based pattern was used to develop cognitive cutpoints and to assess inhabitants frequencies of the totally different preclinical AD levels utilizing totally different cutpoint criteria.
RESULTS
The new criteria subdivide the preclinical section of AD into levels 1 to 3. To classify our CN topics, 2 further classes have been wanted. Stage Zero denotes topics with regular AD biomarkers and no proof of delicate cognitive impairment. Suspected non-AD pathophysiology (SNAP) denotes topics with regular amyloid PET imaging, however irregular neurodegeneration biomarker research. At mounted cutpoints corresponding to 90% sensitivity for diagnosing AD and the 10th percentile of CN cognitive scores, 43% of our pattern was categorized as stage 0, 16% stage 1, 12 % stage 2, 3% stage 3, and 23% SNAP.
CONCLUSIONS
This cross-sectional analysis of the NIA-AA criteria for preclinical AD signifies that the 1-Three staging criteria coupled with stage Zero and SNAP classes classify 97% of CN topics from a population-based pattern, leaving solely 3% unclassified. Future longitudinal validation of the criteria can be vital.

Accuracy of the scientific analysis of Alzheimer illness at National Institute on Aging Alzheimer Disease Centers, 2005-2010.
The neuropathologic examination is taken into account to present the gold normal for Alzheimer illness (AD). To decide the accuracy of presently used scientific diagnostic strategies, scientific and neuropathologic information from the National Alzheimer’s Coordinating Center, which gathers info from the community of National Institute on Aging (NIA)-sponsored Alzheimer Disease Centers (ADCs), have been collected as a part of the National Alzheimer’s Coordinating Center Uniform Data Set (UDS) between 2005 and 2010.
A database search initially included all 1198 topics with not less than one UDS scientific evaluation and who had died and been autopsied; 279 have been excluded as being not demented or as a result of vital information fields have been lacking. The last topic quantity was 919. Sensitivity and specificity have been decided primarily based on “possible” and “potential” AD ranges of scientific confidence and four ranges of neuropathologic confidence primarily based on various neuritic plaque densities and Braak neurofibrillary levels.
Sensitivity ranged from 70.9% to 87.3%; specificity ranged from 44.3% to 70.8%. Sensitivity was usually elevated with extra permissive scientific criteria and specificity was elevated with extra restrictive criteria, whereas the other was true for neuropathologic criteria.
When a scientific analysis was not confirmed by minimal ranges of AD histopathology, essentially the most frequent major neuropathologic diagnoses have been tangle-only dementia or argyrophilic grain illness, frontotemporal lobar degeneration, cerebrovascular illness, Lewy physique illness and hippocampal sclerosis.
When dementia was not clinically identified as AD, 39% of those instances met or exceeded minimal threshold ranges of AD histopathology. Neurologists of the NIA-ADCs had larger predictive accuracy once they identified AD in topics with dementia than once they identified dementing ailments apart from AD. The misdiagnosis price ought to be thought of when estimating topic numbers for AD research, together with scientific trials and epidemiologic research.
